Understanding Hamstring Tendinopathy
Hamstring tendinopathy is a common condition that affects the tendons in the back of your thigh. Understanding the causes, risk factors, symptoms, and diagnosis is crucial for effective management and treatment.
Causes and Risk Factors
Hamstring tendinopathy is usually the result of repetitive stress on the tendons, which can lead to irritation and inflammation (Cleveland Clinic). Several factors can increase your risk of developing this condition:
- Previous Hamstring Injury: The most significant risk factor is a history of previous hamstring injury. The risk of re-injury is 2 to 6 times higher in individuals with a prior hamstring injury.
- Athletic Activities: Athletes or individuals who run at fast speeds, especially those who start and stop quickly, are at the highest risk. This includes sprinters, hurdlers, dancers, and those who play contact sports like football, basketball, or soccer.
- Age: Studies indicate that athletes between 16 and 25 years old are at the highest risk of hamstring injuries.
Symptoms and Diagnosis
Recognizing the symptoms of hamstring tendinopathy is essential for early diagnosis and treatment. Common symptoms include:
- Pain: Pain in the back of your thigh, especially near the buttocks. The pain may worsen with physical activity or prolonged sitting.
- Stiffness: Stiffness in the hamstring area, particularly in the morning or after periods of inactivity.
- Weakness: Weakness in the affected leg, making it difficult to perform activities that involve running or jumping.
- Swelling: Swelling or tenderness in the hamstring region.
To diagnose hamstring tendinopathy, your healthcare provider will perform a physical examination and may recommend imaging tests such as an MRI or ultrasound to assess the extent of the tendon damage.
For more information on related conditions, you can explore our articles on tendinopathy, tendonitis, and gluteal tendinopathy. Understanding these symptoms and risk factors can help you take proactive steps to manage and treat hamstring tendinopathy effectively.
Types of Hamstring Tendinopathy
Chronic High Hamstring Tendinopathy
Characteristics and Symptoms
Chronic high hamstring tendinopathy is a condition that affects the tendons connecting the hamstring muscles to the ischial tuberosity, located at the base of the pelvis.
This condition is often characterized by persistent pain and discomfort in the upper hamstring region, particularly during activities that involve hip flexion and knee extension, such as running, jumping, and sitting for prolonged periods.
Common symptoms of chronic high hamstring tendinopathy include:
- Deep, aching pain in the upper hamstring or buttock area
- Pain that worsens with physical activity, especially running or sitting
- Stiffness and reduced flexibility in the hamstring muscles
- Weakness in the affected leg, leading to difficulty with activities like climbing stairs or standing up from a seated position
Proximal Hamstring Tendinopathy (PHT)
Characteristics and Symptoms
Proximal Hamstring Tendinopathy (PHT) is a chronic overuse injury affecting the tendinous origin of the hamstring muscles at the ischial tuberosity—the bony prominence you sit on at the base of your pelvis.
Unlike general hamstring strains that occur in the muscle belly or lower tendon, PHT specifically involves degeneration and thickening of the proximal tendon, often due to repetitive tensile loading.
It is especially common in distance runners, sprinters, and athletes who perform repeated hip flexion under load, such as during lunges, deadlifts, or prolonged seated positions on hard surfaces (like cycling or rowing).
Key features that make PHT distinct include:
- Deep gluteal or sit-bone pain that is dull or burning in nature, often hard to localize
- Pain that worsens with prolonged sitting, especially on hard surfaces (often called “rower’s butt” or “runner’s butt”)
- Increased discomfort during eccentric hamstring loading, such as during forward lunges, Romanian deadlifts, or uphill running
- Minimal swelling, but clear tenderness when pressure is applied over the ischial tuberosity
- Gradual onset and resistance to healing, due to poor tendon vascularity and ongoing mechanical stress
PHT is often misdiagnosed as sciatica, piriformis syndrome, or ischial bursitis due to the deep buttock pain it causes, making accurate assessment essential for effective treatment.
Treatment Approaches for Hamstring Tendinopathy
These treatment options should be treated as a general guideline, always consult with a healthcare professional for personalized guidance on tendinopathy treatment and medication that is right for you.
Conservative Methods
For many individuals, conservative methods can effectively manage hamstring tendinopathy. One of the most common approaches is the R.I.C.E. method, which stands for rest, ice, compression, and elevation. This method can be done at home to minimize pain and swelling in the hamstring.
Other non-invasive treatments include:
- Heat Therapy: Applying heat to the affected area can help relax and loosen tissues, and stimulate blood flow to the area.
- Stretching: Gentle stretching exercises can help maintain flexibility and reduce stiffness.
- Strengthening Exercises: Focus on exercises that strengthen the hamstring muscles to support recovery.
- Non-Steroidal Anti-Inflammatory Drugs (NSAIDs): Medications like ibuprofen can help reduce pain and inflammation.
- Extracorporeal Shock-Wave Therapy (ESWT): This treatment uses sound waves to promote healing and reduce pain.
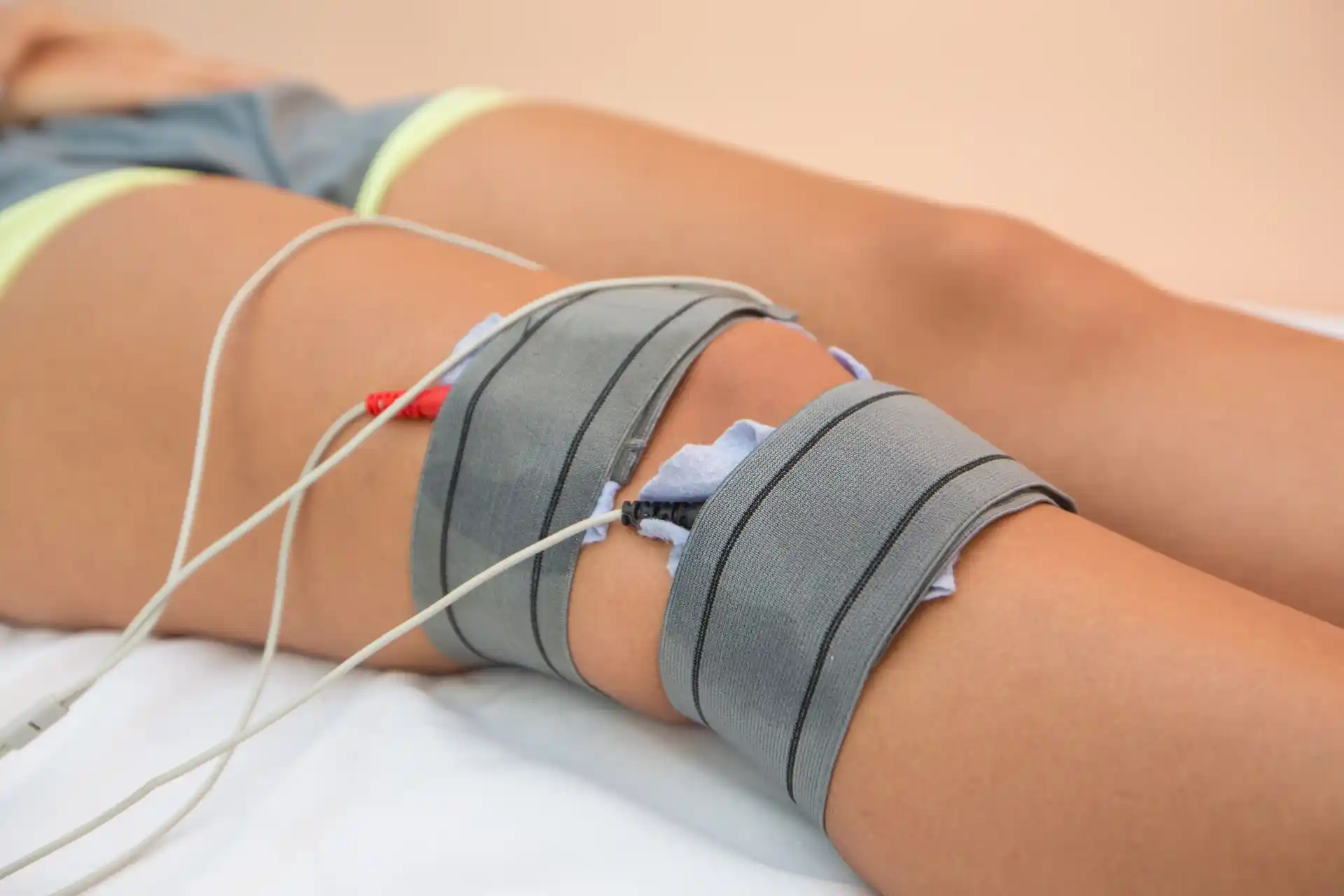
Physical Therapy and Rehabilitation
Physical therapy can be highly beneficial for individuals recovering from hamstring tendinopathy. A physical therapist can design a personalized program to help rebuild strength and flexibility in the leg (Cleveland Clinic).
Key components of physical therapy may include:
- Eccentric Strengthening Exercises: These exercises focus on lengthening the hamstring muscles under tension, which can help prevent new and recurrent injuries.
- Manual Therapy: Techniques such as massage and mobilization can help improve tissue flexibility and reduce pain.
- Functional Training: Exercises that mimic daily activities or sports-specific movements to ensure a safe return to normal activities.
Proper recognition and management of hamstring injuries are crucial for an improved return to sport and a decreased rate of re-injury.
For more information on related conditions, you can explore our articles on proximal hamstring tendinopathy and patellar tendinopathy.
Seek RELIEF®
RELIEF® offers a science-backed, targeted approach to addressing symptoms associated with hamstring tendinopathy.1,2,3,4,5,6,7,8,9
Focusing on treating impacted connective tissue, also known as fascia, that surround the affected tendon to promote healing and enable further support for nearby musculoskeletal structures. RELIEF® is a minimally invasive alternative to traditional treatments—and requires no steroids, medication, surgery, anesthesia, or post-procedure immobilization.
Contact us today to schedule a consultation and learn more about how RELIEF® may help tendinopathy and tendonitis.


.jpg)


.svg)